Angioplasty vs CABG
Best Cardiology Hospital in Mumbai - Angioplasty vs CABG
Let’s try to simplify the conundrum of Angioplasty vs CABG (Coronary Artery Bypass graft surgery) when faced with multi-vessel or Left Main disease with or without LV dysfunction in our patients.
It used to be a fairly simple decision up until a few years ago with all the guidelines suggesting that if someone (with a reasonable life expectancy) has lifestyle limiting angina or suffers a coronary event namely acute coronary syndrome (ACS -STEMI/NSTEMI) and has an angiogram showing Left Main disease / multivessel disease –particularly proximal LAD disease, they should be offered CABG as a superior option as opposed to angioplasty. In the Indian context this also meant an economically better option (a low risk CABG is cheaper than multivessel angioplasty with high quality stents with or without intra-vascular imaging).
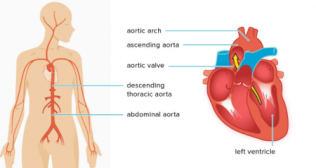
Over the years, the angioplasty world saw several positive and significant changes a “paradigm shift” -- to use a buzz word of the decade. Stents became better and more deliverable, had thinner struts with better polymers or were polymer free and allowed shorter duration of compulsory dual anti-platelet therapy. Some stents need only 1 month of two anti-platelet drugs followed by a low dose Aspirin life-long. Intravascular imaging including IVUS (intra-vascular ultrasound) and OCT (Optical Coherence Tomography) allowed cameras to take detailed pictures from inside the coronaries for accurate determination of the morphology of plaque (calcified vs fibrotic), measurement of the precise lesion length that needed to be stented and the diameter of the stent to be chosen. Post stenting, these high-resolution cameras allow further optimization of the stent result by checking for residual dissections and adequate stent apposition and expansion.
Additionally, advanced and easier techniques to break up the calcium (which used to be the bane of coronary stenting previously) could easily be deployed to prepare the vessel with IVL (Intra-Vascular Lithotripsy-Shock Wave technology) or Orbital atherectomy to complement the vanguard of calcium ablation therapy --Rotablation. These techniques were easier to perform, required a shorter learning curve and were equally effective.
So, for example, if IVUS identified a densely calcific lesion] an appropriate tool such as IVL could be used to break up the calcium with sonic wave energy so that the subsequently deployed stent could be precisely implanted and properly expanded and opposed. All this deployment of tech meant a highly durable and long-term angioplasty result directly competing with what CABG could offer.
All of a sudden, angioplasty became desirable –it didn’t matter if there were multiple stents interventionalists could still use imaging and get long term great results. The attraction of CABG as the sole therapy for long term durable results was being challenged. In the US / Western Europe and South Asian countries (Japan and Korea in particular), patients wanted a 1-2 hour procedure with manageable risks and a very short hospital stay of 2-3 days if there was otherwise equipoise between CABG and stenting.
Trial results between CABG vs PCI in Left Main disease and multi-vessel disease were a mixed bag. While SYNTAX, NOBLE, EXCEL and others showed CABG to be superior vs PCI (mortality benefit), the newer trial with the latest stents -ISCHEMIA trial for example --showed no difference. This is perhaps not all that surprising after all 50% of vein grafts are closed at 5 years. Before the latest iteration of the guidelines, angioplasty was regarded a distant runner-up to CABG in all areas: 3 vessel disease (TVD), Left Main disease and severe LV dysfunction patients.
The guidelines were changed at the 2021 ACC/AHA/SCAI committee meeting and stirred a hornet’s nest.
As far as any Left Main disease and/or multi-vessel disease with severe LV dysfunction was concerned –the guidelines held firm : CABG continued to have a Class I indication (in medical parlance strongly recommended), however for TVD with normal LV function --CABG slipped to a Class 2 b recommendation (weak evidence). Concomitantly, angioplasty now figured in the guidelines as a Class 2 b indication for multi-vessel disease (with preserved LV function) and Class 2 a indication for simple, uncomplicated Left Main disease. Of course, a Heart Team discussion was mandated to ensure that shared decision making with patient preferences were also being given optimal consideration.
The downgrading of CABG in favour of Angioplasty was not without its detractors. There was enough ammunition and statistical parlor tricks to justify one option over the other. Suffice to say, that if the Interventionalist can assure optimal stent outcomes with appropriate imaging and high quality stents, angioplasty can be considered a safe and durable option to CABG. Surgeons should be encouraged to utilize total arterial grafts as conduits, LIMA almost always and RIMA and Radial grafts when possible to really give high quality conduits that will stay open for decades.
Categories
Clear allMeet the doctor

- Cardiac Sciences | Interventional Cardiology
-
22 Years
-
2500