Cor Pulmonale Disease: Causes, Symptoms and Diagnosis
The heart and lungs share a deeply interconnected and codependent relationship. They work in a continuous, elegant loop: the lungs oxygenate the blood, and the heart pumps that oxygen-rich blood to the rest of the body. This partnership is so vital that when one system is under chronic strain, the other is inevitably affected. When long-term lung problems make it difficult for the heart to do its job, it can lead to a specific type of heart failure known as Cor pulmonale.
This condition is not a disease of the heart itself, but rather a consequence of underlying respiratory disease. Understanding this critical link is essential for diagnosis and management, as protecting the heart often means treating the lungs first.
What Is Cor Pulmonale?
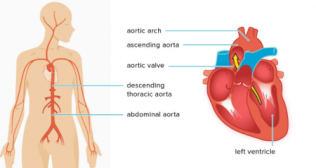
To answer the question, what is Cor pulmonale? It is a medical condition characterized by the enlargement and failure of the right ventricle of the heart. This happens as a direct response to high blood pressure in the pulmonary arteries—the arteries that carry blood from the heart to the lungs. This high pressure is called pulmonary hypertension.
Think of the right ventricle as a pump designed to push blood through the low-pressure system of healthy lungs. When lung disease causes the pressure in the pulmonary arteries to rise, the right ventricle must work much harder to pump against this increased resistance. Over time, this chronic strain causes the muscular wall of the right ventricle to thicken and enlarge (a state called hypertrophy). Eventually, the ventricle becomes so overworked that it can no longer pump blood effectively, leading to right-sided heart failure.
The Underlying Cor Pulmonale Causes
It is crucial to understand that Cor pulmonale is always a secondary condition. The problem does not originate in the heart. The root Cor pulmonale causes are found in diseases that affect either the structure of the lungs or the pulmonary blood vessels themselves.
Chronic Lung Parenchymal Diseases
This is the most common category of causes. These are diseases that damage the lung tissue, leading to scarring and loss of small blood vessels. This increases resistance to blood flow.
- Chronic Obstructive Pulmonary Disease (COPD): Accounting for the majority of cases, COPD (which includes chronic bronchitis and emphysema) causes chronic inflammation and destruction of lung tissue, leading to low oxygen levels and constriction of the pulmonary arteries.
- Interstitial Lung Diseases: Conditions like idiopathic pulmonary fibrosis cause progressive scarring of the lungs, making them stiff and increasing the pressure needed to pump blood through them.
- Cystic Fibrosis: This genetic disorder leads to thick mucus that can damage the lungs over time.
Disorders of the Pulmonary Vasculature
These conditions directly affect the blood vessels of the lungs.
- Chronic Thromboembolic Pulmonary Hypertension (CTEPH): This occurs when blood clots from a pulmonary embolism do not dissolve and instead form organized scar tissue that blocks the pulmonary arteries.
- Primary Pulmonary Hypertension: A rare disease where the pulmonary arteries become narrowed for unknown reasons.
Conditions Affecting Breathing Mechanics
Problems with the chest wall or the nervous system's control over breathing can also lead to low oxygen levels and, eventually, Cor pulmonale.
- Obstructive Sleep Apnea (OSA): Severe, untreated sleep apnea causes repeated drops in oxygen levels during the night, leading to constriction of the pulmonary arteries.
- Severe Kyphoscoliosis: A significant curvature of the spine can compress the lungs and restrict their ability to expand fully.
- Neuromuscular Diseases: Conditions like muscular dystrophy or ALS can weaken the respiratory muscles.
Recognizing the Cor Pulmonale Signs and Symptoms
In its early stages, the Cor pulmonale symptoms are often masked by the symptoms of the underlying lung disease. A person may attribute their increasing shortness of breath to their known COPD, for example.
Early Cor pulmonale signs and symptoms often include:
- Increasing shortness of breath (dyspnea), especially with physical activity.
- A chronic, wet-sounding cough.
- Wheezing.
- Extreme fatigue and lack of energy.
As the right ventricle begins to fail, more specific symptoms of heart failure appear. These occur because the heart can no longer effectively pump blood forward, causing it to back up in the body's veins.
- Peripheral Edema: Swelling in the ankles, feet, and legs.
- Ascites: Swelling in the abdomen due to fluid buildup.
- Jugular Venous Distention: Prominent, bulging veins in the neck.
- Chest Pain (Angina): A feeling of pressure or tightness in the chest, especially during exertion.
- Fainting Spells (Syncope): Particularly with physical activity.
- Cyanosis: A bluish tint to the lips and skin due to low blood oxygen levels.
Diagnosis and Medical Evaluation
Diagnosing Cor pulmonale involves a two-step process: confirming the presence of right ventricular failure and identifying the underlying lung disease causing it. A doctor will use several tools:
- Physical Examination: A doctor will listen to the heart and lungs and look for physical signs like leg swelling and prominent neck veins.
- Echocardiogram: This is a key diagnostic test. It is an ultrasound of the heart that allows the doctor to see the size and function of the right ventricle and to estimate the pressure in the pulmonary arteries.
- Blood Tests: These are used to measure oxygen levels and to check for a hormone called BNP, which is elevated when the heart is under strain.
- Chest X-ray or CT Scan: These imaging tests can show enlargement of the right ventricle and pulmonary arteries and can help diagnose the underlying lung disease.
- Electrocardiogram (ECG): This test can detect abnormal heart rhythms and signs of right ventricular hypertrophy.
- Right Heart Catheterization: This is the most accurate method for measuring the pressure inside the right ventricle and pulmonary arteries. A thin tube is guided through a vein into the heart.
A Focus on Comprehensive Care
Cor pulmonale is a serious condition that undersCores the critical relationship between our respiratory and cardiovascular systems. It serves as a powerful reminder that the health of the lungs has a direct and profound impact on the heart.
Effective management requires a comprehensive approach that focuses on treating the underlying lung disease to reduce the strain on the heart. Through diligent care and a proactive partnership with your healthcare team, it is possible to manage symptoms and improve your overall quality of life.
Frequently Asked Questions
1. Can Cor pulmonale be cured or reversed?
Ans. The heart failure itself cannot be cured, but its progression can be slowed or halted by effectively treating the underlying lung condition. If the lung disease is managed well, the strain on the heart can be significantly reduced.
2. What is the life expectancy for someone with Cor pulmonale?
Ans. Life expectancy varies greatly and depends almost entirely on the severity and management of the underlying lung disease, not the heart failure itself.
3. Is Cor pulmonale the same as congestive heart failure?
Ans. It is a type of heart failure, but "congestive heart failure" usually refers to left-sided heart failure. Cor pulmonale specifically refers to right-sided heart failure caused by lung problems.
4. How is the treatment different from other types of heart failure?
Ans. The primary focus of treatment is on the lungs. While supportive heart medications may be used, the main goal is to improve lung function and lower pulmonary artery pressure.
5. Can lifestyle changes help manage Cor pulmonale?
Ans. Yes. Quitting smoking is the single most important step. Following your doctor's advice for oxygen therapy, managing fluid intake, and engaging in pulmonary rehabilitation can all make a significant difference.