Don’t Miss the Signs: Understanding the Danger of Aortic Dissection
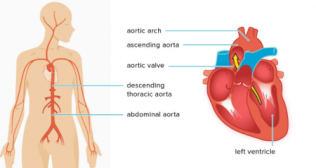
The aorta is the largest and most important artery in the body, a superhighway for blood that originates from the heart and extends down through the chest and abdomen. Its thick, resilient walls are built to withstand the immense pressure of every heartbeat. However, when a tear occurs in the inner layer of this mighty vessel, it can lead to a catastrophic and often fatal medical event known as an aortic dissection.
This condition is one of the most serious emergencies in cardiovascular medicine. It is a race against time, where immediate recognition of the symptoms and prompt medical intervention are the only things that stand between life and death. Understanding this silent but deadly condition is crucial for both patients at risk and the public at large.
What Is an Aortic Dissection?
An aortic dissection is a tear that occurs in the innermost layer of the aorta's wall (the tunica intima). When this tear happens, high-pressure blood surges through it, forcing its way between the inner and middle layers of the artery wall. This creates a new, false channel for blood flow. As the blood continues to pump, it can cause this channel to extend further along the length of the aorta, "unzipping" the layers as it goes.
This process is dangerous for two main reasons. First, it weakens the outer wall of the aorta, putting it at risk of a complete rupture, which leads to massive internal bleeding and is almost always fatal. Second, the false channel can compress the true channel or block off the smaller branch arteries that supply blood to vital organs like the brain, heart, kidneys, and spinal cord.
The Underlying Aortic Dissection Causes
The primary trigger for an aortic dissection is a chronic weakening of the aortic wall. The most significant and common of all aortic dissection causes is long-term, uncontrolled high blood pressure (hypertension). The constant strain on the artery wall can lead to degeneration of its tissues, making it more prone to tearing.
Other Major Risk Factors
- Genetic Conditions: Certain inherited connective tissue disorders significantly weaken the aorta. Marfan syndrome is the most well-known, but others include Ehlers-Danlos syndrome and Loeys-Dietz syndrome.
- Pre-existing Aortic Conditions: Individuals with a known thoracic aortic aneurysm (a bulge in the aorta) are at a much higher risk. Bicuspid aortic valve, a congenital heart defect, also increases the risk.
- Atherosclerosis: While not a direct cause, severe hardening of the arteries can contribute to the weakening of the aortic wall.
- Trauma: A severe blow to the chest, such as from a major car accident, can cause a traumatic aortic dissection.
- Age: The risk increases with age, with most cases occurring in people in their 60s and 70s.
Recognizing the Critical Aortic Dissection Symptoms
The aortic dissection symptoms are typically sudden, severe, and often described as unlike any pain ever experienced before. Recognizing these signs is the most critical factor in survival.
The Classic Symptom
- Sudden, Severe, Tearing or Ripping Pain: This is the hallmark symptom. The pain is often felt in the chest or upper back and is frequently described as a sharp, tearing, or ripping sensation. The location of the pain may migrate as the dissection extends along the aorta.
Other Important Symptoms
- Shortness of Breath: Difficulty breathing can occur if the dissection affects the aortic valve or causes fluid to back up into the lungs.
- Symptoms of a Stroke: If the dissection disrupts blood flow to the brain, it can cause stroke-like symptoms, such as sudden weakness or paralysis on one side of the body, difficulty speaking, or loss of vision.
- Loss of Consciousness (Syncope): A sudden fainting spell can be a sign of a critical drop in blood pressure.
- Weak Pulse in One Arm: A noticeable difference in the pulse or blood pressure between the right and left arms is a classic clinical sign.
- Leg Pain or Paralysis: If the dissection extends down into the abdominal aorta and blocks blood flow to the legs or spinal cord.
The Types of Aortic Dissection
The location of the initial tear determines the type of dissection and the urgency of the treatment. The Stanford classification is the most commonly used system.
Type A Aortic Dissection
A type A aortic dissection is the more common and far more dangerous type. It involves a tear in the ascending aorta, the part of the aorta that rises out of the heart. This type is a surgical emergency because it can easily rupture or extend backward to affect the heart's coronary arteries or the aortic valve, leading to a heart attack or acute heart failure.
Type B Aortic Dissection
A type B aortic dissection involves a tear only in the descending aorta, the part that travels down through the chest and abdomen. While still very serious, this type is often managed initially with aggressive medical therapy rather than immediate surgery.
The Role of Aortic Dissection Radiology in Diagnosis
When a patient presents with symptoms of a dissection, a rapid and accurate diagnosis is essential. The field of aortic dissection radiology is central to this process.
CT Angiography (CTA): This is the gold standard and the most widely used imaging test. It is fast, highly accurate, and can clearly show the tear, the false lumen, and any involvement of branch arteries.
Transesophageal Echocardiogram (TEE): This is an ultrasound probe that is passed down the esophagus to get a very clear, close-up view of the aorta. It is particularly useful for unstable patients who cannot be moved to a CT scanner.
The Urgent Aortic Dissection Treatment
The treatment strategy is dictated by the type of dissection.
For a Type A Aortic Dissection: The only treatment is immediate, life-saving open-heart surgery. The goal of the aortic dissection treatment is to remove the torn section of the ascending aorta and replace it with a synthetic graft.
For a Type B Aortic Dissection: The initial treatment is aggressive medical management in an intensive care unit (ICU). This involves powerful medications to lower the blood pressure and heart rate, which reduces the stress on the aortic wall. Surgery or a less invasive procedure called TEVAR (Thoracic Endovascular Aortic Repair) is reserved for cases with complications, such as a rupture or lack of blood flow to vital organs.
A Matter of Minutes
An aortic dissection is a true medical emergency where the risk of death increases with every passing hour. The key to survival is the immediate recognition of its unique, severe symptoms and seeking emergency medical help without delay.
For those with known risk factors, the most powerful tool is prevention. Meticulously controlling high blood pressure and undergoing regular screening for aortic aneurysms can stop this catastrophic event before it ever has a chance to begin.
Frequently Asked Questions
1. Can you survive an aortic dissection?
Yes, but survival is highly dependent on getting immediate medical treatment. For a Type A dissection, the risk of death is about 1-2% per hour for the first 48 hours. With prompt surgery, survival rates are much higher.
2. What does the pain of an aortic dissection feel like?
It is most often described as a sudden, maximal, tearing or ripping pain in the chest or back, between the shoulder blades. It is very different from the pressure-like pain of a heart attack.
3. Is an aortic dissection the same as an aneurysm?
No. An aneurysm is a bulge or swelling in the aorta's wall. A dissection is a tear in the wall's inner lining. However, having an aneurysm is a major risk factor for a future dissection.
4. How long does the surgery for a Type A dissection take?
It is a long and complex open-heart surgery that can take anywhere from 4 to 8 hours or even longer, depending on the extent of the damage.
5. What is the recovery like after surgery?
Recovery is similar to other major open-heart surgeries, involving several days in the ICU followed by a longer hospital stay. Full recovery can take several months.