Hyperlipidemia: Know About Its Causes and Symptoms
Some of the most significant threats to our long-term health are the ones we cannot see or feel. These are the silent conditions, those that develop quietly over years without sending out any warning signals until serious damage has already been done. One of the most common and consequential of these is hyperlipidemia, a medical term that might sound complex but refers to a very straightforward and manageable issue: high levels of fats in the blood.
Understanding this condition is the first and most critical step in protecting your cardiovascular health for the future. Receiving a diagnosis can be unsettling, especially when you feel perfectly fine. However, this knowledge is a powerful tool, empowering you to make proactive choices that can dramatically reduce your risk of heart disease and stroke down the road.
What Exactly Is Hyperlipidemia?
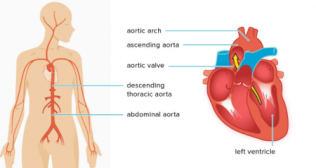
To understand hyperlipidemia, let's break down the word. "Hyper" means high or elevated, and "lipidemia" refers to the lipids, or fats, circulating in your bloodstream. So, the term simply means you have high levels of these fats, which primarily include cholesterol and triglycerides.
While your body needs a certain amount of these lipids to function correctly, building cells and creating hormones, too much of a good thing can become dangerous. Think of your blood vessels as a complex plumbing system.
Low-Density Lipoprotein (LDL): This is often called the "bad" cholesterol. Imagine it as a sticky, waxy substance. When you have too much LDL, it can build up on the inner walls of your arteries, forming a thick, hard substance called plaque. This process is called atherosclerosis.
High-Density Lipoprotein (HDL): This is the "good" cholesterol. Think of HDL as the cleanup crew for your plumbing system. It travels through your arteries, collects excess cholesterol, and transports it back to the liver, where it is removed from the body.
Triglycerides: This is another type of fat found in your blood that your body uses for energy. Excess calories, especially from sugar and alcohol, are converted into triglycerides and stored in fat cells. High levels can also contribute to the hardening of the arteries.
Hyperlipidemia is the state of having too much LDL or triglycerides, not enough HDL, or a combination of these issues.
The Common Hyperlipidemia Causes You Should Know
The reasons why a person develops high lipid levels fall into two main categories. It is often a combination of both that leads to the condition. Understanding the hyperlipidemia causes can help you and your doctor formulate the best management plan.
Primary or Familial Hyperlipidemia
This type is genetic. Some people inherit genes from their parents that cause their bodies to produce too much LDL cholesterol or make it difficult for the body to remove it from the blood. This can lead to very high cholesterol levels even in people who are young, physically fit, and follow a healthy diet. It is a powerful reminder that you cannot always judge your risk based on your appearance or lifestyle alone.
Secondary or Acquired Hyperlipidemia
This is the most common form and is directly influenced by lifestyle factors and other underlying medical conditions. The choices we make every day, and our overall health status play a huge role in our lipid levels. Key factors include:
Diet: A diet high in saturated fats (found in red meat, full-fat dairy, and butter) and trans fats (found in many processed and fried foods) can significantly raise your LDL cholesterol.
Sedentary Lifestyle: A lack of regular physical activity can lower your protective HDL cholesterol levels.
Obesity: Being overweight or obese is strongly linked to higher levels of LDL and triglycerides and lower levels of HDL.
Underlying Health Conditions: Certain diseases can disrupt the body's ability to manage lipids, including type 2 diabetes, chronic kidney disease, and an underactive thyroid (hypothyroidism).
Certain Medications: Some drugs, such as certain types of blood pressure medications and steroids, can affect lipid levels as a side effect.
The Silent Nature of Hyperlipidemia Symptoms
This is the most crucial point to understand about the condition. In the vast majority of cases, hyperlipidemia has absolutely no symptoms. You cannot feel that you have high cholesterol. It does not cause headaches, fatigue, or any other noticeable signs in its early stages. This is why it is often called a silent threat.
People can live for years or even decades with dangerously high lipid levels and be completely unaware. This applies to all age groups, so the symptoms of hyperlipidemia in adults are typically absent. The danger is that during this entire symptom-free period, plaque can be slowly and steadily building up in the arteries, narrowing them and making them less flexible.
When Symptoms Do Appear
Hyperlipidemia symptoms only emerge when the underlying atherosclerosis has become so advanced that it is restricting blood flow to vital organs. These are not symptoms of hyperlipidemia itself, but rather symptoms of the severe cardiovascular disease it has caused. These can include:
Chest Pain (Angina): A sign that the heart muscle is not getting enough oxygen-rich blood.
Shortness of Breath: Can also indicate a problem with heart function.
Leg Pain When Walking: Known as claudication, this is a symptom of peripheral artery disease (PAD), where the arteries supplying blood to the legs have narrowed.
Heart Attack or Stroke: These are often the first, and most catastrophic, sign that a person has had untreated hyperlipidemia for a long time.
How This Condition Is Diagnosed
Because of its silent nature, the only reliable way to know if you have hyperlipidemia is through a simple blood test called a lipid panel or lipid profile. This test, usually done after a 9-to-12-hour fast, measures your total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides.
Regular screening is essential for early detection and prevention. Your doctor can recommend how often you should be tested based on your age, family history, and other risk factors for heart disease. This simple blood test provides a clear picture of what is happening inside your arteries.
An Overview of Hyperlipidemia Treatments
A diagnosis of hyperlipidemia is not a life sentence. It is a highly manageable condition, and taking control of it is one of the most important things you can do for your long-term health. The main hyperlipidemia treatments involve a two-pronged approach.
Lifestyle Changes Are the Foundation
For many people, lifestyle modifications are the first line of defense and the cornerstone of any treatment plan. These changes include:
A Heart-Healthy Diet: Reducing your intake of saturated and trans fats while increasing your consumption of soluble fiber (from oats, fruits, and vegetables) and healthy fats (from avocados, nuts, and olive oil).
Regular Physical Activity: Aiming for at least 150 minutes of moderate-intensity exercise, like brisk walking, per week can help raise HDL and lower LDL and triglycerides.
Weight Management: Losing even a small amount of weight can have a significant positive impact on your lipid levels.
Quitting Smoking: Smoking damages blood vessels and lowers HDL cholesterol, making it a major risk factor.
The Role of Medication
When lifestyle changes alone are not enough to reach your target lipid levels, your doctor may prescribe medication. The most common and effective class of drugs for lowering LDL cholesterol is statins. These medications work by reducing the amount of cholesterol your liver produces. Other medications may be used to lower triglycerides or raise HDL.
Your Proactive Partner in Heart Health
Hyperlipidemia is a perfect example of a silent condition where knowledge and prevention are your strongest allies. Since it rarely presents with clear symptoms, regular blood tests are the only way to detect it early and prevent its progression to serious disease.
Knowing your cholesterol numbers is just as important as knowing your blood pressure. Partner with your healthcare provider to understand your individual risk, get screened regularly, and develop a personalized plan to keep your heart and blood vessels healthy for a lifetime.
Frequently Asked Questions
Q1. How often should I get my cholesterol checked?
Ans. Guidelines suggest that healthy adults with no other risk factors should have their cholesterol checked every four to six years. However, if you have risk factors like a family history of high cholesterol, heart disease, diabetes, or obesity, your doctor will likely recommend more frequent testing.
Q2. Can thin or athletic people have high cholesterol?
Ans. Yes, absolutely. This is a common misconception. While obesity and a sedentary lifestyle are major risk factors, your genetics play a powerful role. A person can be very fit and still have high cholesterol due to familial hyperlipidemia, which is why screening is important for everyone.
Q3. Are high triglycerides as dangerous as high LDL cholesterol?
Ans. Very high triglyceride levels are a significant risk factor for pancreatitis and are also considered an independent risk factor for atherosclerosis and heart disease. While LDL is often the primary focus, managing high triglycerides through diet, exercise, and sometimes medication is also a crucial part of reducing cardiovascular risk.
Q4. Can I stop my medication once my cholesterol is normal?
Ans. No. You should never stop taking a prescribed cholesterol medication without first consulting your doctor. These medications work by continuously managing your body's cholesterol production. If you stop taking them, your cholesterol levels will almost certainly rise again.